Brain Injury Rehabilitation: From Injury to Recovery
Four things to know along the way
More than 5.3 million individuals in the United States live with a permanent brain injury-related disability.
That's one in every 60 people, according to the Brain Injury Association of America.
Every brain injury is unique and so is the outlook for recovery.
Chances for recovery depend on many things. Severity of injury is the biggest factor. But the type of injury, age and health are factors too.
An individual's recovery happens in stages and recovery time will vary from person to person.
For families and caregivers, understanding the recovery process can help set expectations. To better understand brain injury and recovery, this blog will share:
- Types of brain injury and their impact
- How a personalized care plan increases the chances of recovery
- Who is on a brain injury care team and what they do
- The power of inpatient brain injury rehabilitation for a better recovery
Read on to see what recovery may look like with brain injury rehabilitation.
What is a brain injury and its impact?
Brain injuries are either traumatic or non-traumatic.
Traumatic brain injuries (TBIs) result from an outside force to the head (e.g., hitting the head in a fall or a car accident). The primary impact of TBI is bruising which can damage the brain. There is also a chance of damage to the nerves, brain tissue and blood vessels.
Secondary impacts can occur from bleeding in the brain, causing headaches and swelling.
Non-traumatic brain injuries are from an internal cause like a brain tumor or blood clot.
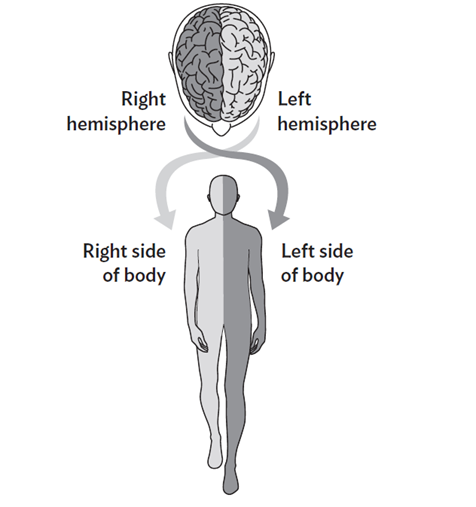
Whether TBI or non-traumatic, the impact of a brain injury depends on the side of the brain affected.
With a left-brain injury, weakness typically shows on the body's right side.
The opposite is true for right-brain injuries. Weakness is on the body's left side. In either case, the weakness stems from the brain’s inability to process sensory signals in the body in the right way.
That’s where the similarities end.
People who have left-brain injuries may have trouble finding their words. They may not understand the words they hear.
With right-brain injuries, attention span may wane. Memory or reasoning may fail. Right-brain injury can impair the ability to control their behavior or what they say. Download our Left Brain, Right Brain Controls infographic.
Recovery from brain injury is complex and it’s different for all patients.
But in all cases, brain injury rehabilitation can help restore function and ability.
Brain injury rehabilitation and its role in recovery
Rehabilitation is key in helping injured people recover to their fullest ability. Brain rehabilitation therapy helps with relearning function lost as a result of a brain injury.
— Mayo Clinic
Brain injury rehabilitation often starts in an acute care hospital.
Many patients then move to an inpatient rehabilitation setting, like ours.
We work with the teams at acute care hospitals for a smooth transition to our program.
We do an assessment to create a personal care plan for each patient. This starts the next stage of recovery.
The assessment ensures a patient can do a five-day-a-week schedule of therapy. Each day includes three hours of therapy.
The care plan is a roadmap for therapy that is followed throughout the patient's stay.
Rehabilitation works to improve quality of life. That means helping patients progress through the stages of recovering brain function. The goal is to help them regain their abilities to their fullest potential.
“Take advantage of the rehab and make the most out of the experience. It’s the best way to return to how you were before the injury.”
— Nolan Broughton, former TBI patient
Your brain injury care team
Creating a rehabilitation and recovery plan for brain injury is a team effort.
That team is led by a physiatrist. This is a doctor who specializes in physical medicine and rehabilitation.
The team can include:
- Nurses who specialize in rehabilitation. They give medications and track vital signs. They also help lift, turn and safely move patients in and out of bed and within the hospital room.
- Physical therapists who work to improve a patient's balance, mobility and strength. This takes place with daily structured physical activity.
- Occupational therapists who teach patients new ways to do daily living tasks. This includes toileting, bathing and dressing.
- Speech and language therapists who assess swallowing and speech. They also help with cognitive issues of memory, concentration and learning.
- Dietitians who help with nutrition. They educate patients and families on special diets prescribed and food preparation.
- Psychologists/neuropsychologists* who assess and treat mental, social or emotional health needs. This can help with coping skills and managing stress.
*Not available at all SSM Health Rehabilitation Hospitals.
Our approach centers on patient wholeness – medical, physical, mental, emotional health. This helps each person reach their maximum potential.
“My therapists never let me back down. The stronger I got, the better I felt.”
— James Weiss, former TBI patient
Brain injury recovery is a long journey. It’s important to know that not all patients will recover to full independence when they leave us.
That’s why we provide patient and caregiver education on ways to adapt certain tasks. This may include training on the safe use of a wheelchair or walker in home. It can also guide the patient on how to safely return to activities and family involvement.
Before discharge, we’ll identify special needs, like home health care, for continued recovery once the patient has left the hospital.
Benefits of brain injury rehabilitation at SSM Health Rehabilitation Hospital
Specialized brain injury rehab is not available in all care settings.
Our scope of services can more fully treat the varying types and degrees of brain injury.
In short, our team approach can address wider impacts on the brain and set the right road to recovery. This is good news for patients who are medically able to take part in rehab.
Cognitive/thinking skills
After traumatic brain injury, patients can suffer changes in thought patterns. They can experience something called mental fatigue or “brain fog.”
In such cases, changing the therapy environment can help the patient focus. This can be a quiet room instead of a busy therapy gym.
Patients with less severe injury may not need a change in environment. Rather, they have the ability to concentrate but could have trouble with problem-solving.
Here, therapy may include using numbers or math skills. This can help in relearning tasks like bill paying or medication management.
Behavior management
Brain injury may cause confusion or extreme agitation. Either of these can impact behavior.
It could mean impaired judgment -- an inability to control what they do or say. One individual may be emotional while another may withdraw or be emotionless. Others may be hostile or violent.
Changes in behavior signal damage to the frontal lobe. This part of the brain controls expression and behavior.
Disruptive behavior is hard for patients and families. Here, too, a team approach is better in treating diverse impacts of brain injury.
Muscle weakness
There is an expression that we are “hard-wired” to do things.
Throughout life, the brain changes. It adapts to new experiences using those “wired” connections to learn.
But like electrical wiring, those connections can be severed by illness or injury. For instance, a brain injury can change muscle tone.
Muscle tone, or the amount of tension in the muscle, can become low (floppy) or high (tight or stiff). Both result from injury to areas of the brain that control how muscles tighten and relax.
A patient may want to move the hands or feet but the thought doesn't connect with the brain. To rebuild muscle tone and regain function means the brain must form new connections.
Called neuroplasticity, it's a rewiring -- retraining -- of the brain to relearn an action.
In therapy, we use a range of activities to help with this rewiring. This retrains the connection between brain and body.
Neuroplasticity therapy can include:
- Repetitive practice of daily activities
- Therapeutic exercises like balance and strength training
- Manual therapy, such as stretching and massage
Vision problems
Vision problems can occur with brain injury. In these cases, occupational therapists will assess any visual issues.
Common ones include loss of peripheral vision (one or both eyes) and double vision.
There may also be an inability to make sense of what the eyes see. Think of puzzle pieces and not being able to put them together.
Therapists help patients work through visual issues to help the brain make sense of what the eyes see.
Speech, Language and Swallow Disorders
A speech-language pathologist will assess any changes in communication and swallowing.
For trouble in these areas, therapy is a training aid for learning different ways to talk and respond. These may be using:
- Simpler phrases
- Yes/no questions
- Gestures to help with meaning
- Oral exercises and breathing techniques to improve speaking ability
Outside of speech therapy, food preparation is key for trouble chewing and swallowing. Usually, this is a change in food texture (e.g., pureed or thickened liquids) for safe swallowing when eating or drinking.
Brain injury rehabilitation is lengthy. But it is a way forward for survivors, their friends, families and caregivers.
For those living with a brain injury, there is hope and help for patients to grow their skills and rebuild their lives.
“I grew by leaps and bounds in rehab.”
— David Volman, former TBI patient
For more hope and inspiration, read the recovery stories of our brain injury patients.